Part 1: Unraveling Healthcare Waste: Administrative Challenges and Expenses
Abstract:
In an analysis presented as the cornerstone of a comprehensive six-part examination, we navigate the intricate landscape of healthcare spending and administrative challenges that presently define the American healthcare system. This discourse, positioned at the juncture of rising costs and a complex administrative framework, sheds light on the sector's struggle with inefficiencies that significantly inflate expenditures, amounting to an estimated $265.6 billion in wasteful spending. With healthcare expenses reaching $4.3 trillion, or an average of $12,900 per individual, the industry grapples with balancing the provision of premier care against the backdrop of escalating administrative duties. These duties not only burgeon costs but also potentially compromise the quality of patient care. The analysis traverses the domain of hospitals, insurance entities, and healthcare facilities, where administrative burdens vie for resources, precipitating heightened insurance premiums and out-of-pocket costs for insured parties. Inaugurating with a historical overview of healthcare spending vis-à-vis economic trends, the narrative embarks on a journey through the financial dynamics at play within the healthcare industry. It highlights a critical exploration of the burgeoning costs shouldered by both employers and employees, alongside the personal financial strains experienced by individuals and families. At the core of our investigation lies the often-underestimated realm of administrative tasks. These tasks, identified as a major source of inefficiency, not only elevate costs but also detract from the essence of patient care. Our exposition culminates in the proposition of innovative strategies aimed at dismantling the complexities of administrative processes, thereby curbing unnecessary expenditures. Through this series, we aspire to offer insightful context, dissect the multifaceted financial pressures plaguing the system, and chart a course toward a more efficient and equitable healthcare landscape.
Author:
Aldo M. Martinez, MBA, MPA
A: Introduction
The state of healthcare in America is at a turning point, teetering between rising costs and the complex web of administrative challenges—administrative complexity accounts for $265.6 billion in wasteful costs, according to a study published in JAMA.[i] According to data, the healthcare sector spent $4.3 trillion, averaging $12,900 per person.[ii] While healthcare providers are dedicated to delivering top-notch care to patients, they are faced with a battle against the increasing administrative tasks that inflate costs and could potentially impact the quality of care. In the world of hospitals, insurance offices, and clinic front desks, these administrative burdens compete for resources, leading to higher premiums and out-of-pocket expenses for those with insurance. This puts pressure on both the system's sustainability and the public's finances. In this article, the inaugural piece of a comprehensive six-part series, we undertake a thorough examination of historical healthcare spending trends and delve into the intricacies of the sector's financial dynamics, offering a backdrop of insightful context. We will then explore escalating costs imposed on both employers and employees, while also illuminating the financial pressures that individuals and families face. Concluding our exploration, we will scrutinize administrative tasks—a substantial, yet often overlooked fount of inefficiency—assessing their toll on patient care and overall healthcare results. Our analysis will culminate with a look at forward-thinking strategies aimed at simplifying administrative processes and curbing wasteful expenditure.
B: Contextual Information on Healthcare Spending
Looking Back at Economic Stability and Healthcare Spending Trends
In the United States, 18 percent of the gross domestic product (GDP) is attributed to healthcare costs.[iii] The US spends more on healthcare than any other country in the world.[iv] “Prior studies estimated that approximately 30% of health care spending may be considered waste.”[v] Between 2010 and 2019, the growth in healthcare spending closely mirrored the economic growth, showing a slight increase of 0.3 percentage points compared to the GDP's growth.[vi],[vii] See Figure 1. This contrasts with the decade when healthcare spending outpaced GDP growth by 3.0 percentage points until the Affordable Care Act was implemented.[viii] Historically, significant disparities between healthcare spending and economic growth have often triggered government interventions, leading to widespread healthcare reforms, particularly during times of economic downturn.[ix] See Figure 2.
Figure 1: Adapted from The Gathering Storm: The Uncertain Future of U.S. Healthcare." McKinsey & Company. September 16, 2022.
Figure 2: Adapted from The Gathering Storm: The Uncertain Future of U.S. Healthcare." McKinsey & Company. September 16, 2022.
Exploring the Financial Dynamics of the Healthcare Industry
The question at hand concerns the strategies that stakeholders such as businesses, individual clients, and public institutions will employ to manage escalating expenses, a scenario that potentially endangers the sector's profitability, specifically its earnings before interest, taxes, depreciation, and amortization (EBITDA).[x] The factors mentioned earlier could put at risk over half of the total profit by 2027, amounting to approximately $450 billion.[xi], [xii] Nonetheless, the healthcare sector presents an opportunity for enhancement valued at $1 trillion.[xiii] This opportunity provides a path toward improving healthcare overall and alleviating potential pressures on profit margins.
Increasing Burden of Healthcare Expenses on Employers and Employees
Employers are increasingly transferring the financial burden related to healthcare costs onto their employees. The shift towards deductible health plans reflects a changing landscape, as enrollment in such plans has “more than doubled from 18 percent in 2013 to 40 percent in 2021.”[xiv] This means employees spend more on out-of-pocket expenses for their healthcare needs. Moreover, an “overwhelming majority of companies (95 percent) indicated their readiness to modify benefit schemes should cost hikes exceed 4 percent.”[xv] The move towards increased cost-sharing by employees signifies a reassessment of benefit packages by employers due to escalating costs, indicating possible hurdles ahead for both employers and employees in managing healthcare expenses.
The Financial Strain on Individuals
The financial impact of healthcare on individuals has become more evident over time. Data from “2021 reveals a financial landscape for many American households, with out-of-pocket healthcare expenses averaging between $8,000 and $12,000 per year.”[xvi] Given that the average household savings in 2021 stood at $20,000, the consumer's ability to manage these costs is constrained.[xvii]
Adding to the complexity of this situation is the occurrence of medical debt, with “22 percent of individuals disclosing that they owe more than $1,000 in medical bills.”[xviii] “34 percent mention affordability as the main reason for delaying essential healthcare, while 45 percent would opt to skip a doctor’s appointment over a mere $10 cost increase.”[xix] The choice to postpone medical attention due to financial concerns, as well as the sensitivity to even minor price hikes, highlights the financial strains consumers face. Despite wage hikes, real earnings have been affected by inflation, making healthcare less affordable and accessible.[xx]
Predicted Surge in Healthcare Expenditure
Looking into the future, estimates indicate a rise in healthcare spending compared to overall economic growth. Between 2022 and 2027, healthcare costs are projected to grow at a rate of 7.1 percent, surpassing the expected economic growth rate of 4.7 percent.[xxi] See Figure 3. This widening disparity underscores the mounting pressure on the healthcare system due to factors like high inflation rates, ongoing shortage of medical personnel, and sluggish economic growth.[xxii]
Figure 3: Adapted from The Gathering Storm: The Uncertain Future of U.S. Healthcare." McKinsey & Company. September 16, 2022.
C. Administrative Complexity and Wasteful Spending
Understanding Administrative Complexity
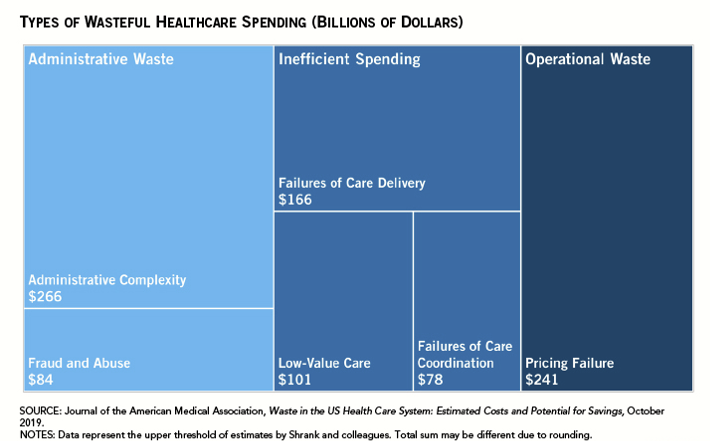
In the realm of healthcare, administrative complexity often appears as an intricate and constantly shifting puzzle, where each piece represents a segment of the overarching system. At the forefront, hospitals grapple with elaborate billing systems; insurance companies contend with stringent policy approval sequences; and clinics manage the nuanced demands of patient care coordination. Though integral to healthcare fabric, these components can often weave a web of inefficiency. Shrank et al. pinpoint this administrative entanglement as the source of an estimated “$265.6 billion in wasteful spending, accounting for a significant slice of healthcare spending in the United States.”[xxiii] See Figure 4. In 2021, the United States spent “$1,055 per capita on such costs, while the second highest level of such spending was Germany at $306 per capita. That difference is partially due to the administrative complexity of having multiple payers in the U.S. healthcare system.”[xxiv] This magnitude of waste not only siphons off funds but also diverts the healthcare system's gaze from its primary focus on patient care.
Figure 4: As quoted in Peter G. Peterson Foundation. "Almost 25 Percent of Healthcare Spending Is Considered Wasteful — Here's Why." Peter G. Peterson Foundation. 2023
Within the operational cores of these institutions, the maze intensifies. Hospitals struggle with labyrinthine billing procedures, insurance companies with the quagmire of policy reviews and denials, and clinics with an increasing heap of regulatory mandates.[xxv] This expansion of bureaucracy calls for a disproportionately large allocation of resources to administrative functions, drawing them away from patient services. As outlined by The American Journal of Managed Care, the ballooning of operational expenses directly affects the cost to patients, manifested in rising healthcare premiums and co-payments.[xxvi] This trend continues, fueling a cycle where escalating costs do not equate to improved quality of patient care.
Impact on Healthcare Costs and Patient Outcomes
In the sprawling ecosystem of U.S. healthcare, administrative costs loom large, casting long shadows over budgets and bedside manners alike. For every intricate billing procedure, every meticulous insurance policy review, and each precise patient management protocol, there is a price — and it's not just measured in dollars and cents. This financial hemorrhage diverts the focus from where it should be — on patient care — to the intricate web of administrative tasks.
This investment in administrative architecture impacts the very core of healthcare delivery. Hospitals and clinics, in their pursuit of navigating this complex structure, end up channeling a disproportionate amount of resources toward administrative upkeep rather than towards enhancing patient care. The intricate administrative procedures in America's healthcare framework play a major role in the rising costs for those who provide care. This, in turn, trickles down to everyday people who find themselves paying more in health insurance premiums and their share of medical bills.[xxvii] This financial upswing, however, does not necessarily equate to an uptick in care quality. The steep costs associated with administrative complexity are also echoed in the time invested by physicians, where handling billing-related matters is estimated to cost around $68,000 per physician each year.[xxviii] Such figures are not merely abstract numbers; they represent a profound investment of time and resources that could otherwise be channeled toward patient care and improved health outcomes. This shift is palpable in-patient satisfaction and care quality as “excessive administrative tasks divert time and focus from more clinically important activities of physicians and their staffs, such as providing actual care to patients and improving quality, and may prevent patients from receiving timely and appropriate care or treatment.”[xxix]
Innovative Solutions to Reduce Administrative Complexity
In the pursuit of streamlining the healthcare labyrinth, the industry is turning to inventive strategies to pare down administrative complexities. The advent of value-based care models marks a pivotal shift, as they underscore the quality of patient outcomes rather than the number of services rendered, thus cutting through the administrative tape that binds traditional fee-for-service frameworks. Likewise, the integration of care systems emerges as a promising solution, unifying diverse healthcare services under a consolidated administrative structure to enhance care and reduce bureaucratic layers.
Technological innovations are revolutionizing healthcare operations. Implementing Electronic Health Records (EHRs) has been pivotal in improving care coordination across healthcare delivery organizations, fostering a more interconnected and patient-centric approach.[xxx],[xxxi] Electronic Health Records (EHRs) significantly improve the way healthcare professionals collaborate by creating a system that is efficient and centered on patient needs. Research by Adler-Milstein et al. found that EHR systems share patient data between teams, clinical departments, and even between different healthcare providers more efficiently; therefore, increasing the quality of patient care and healthcare costs decrease.[xxxii] Further, artificial intelligence tools are empowering insurance companies to expedite claim processing, elevating efficiency and accuracy.
The 2009 enactment of the Health Information Technology for Economic and Clinical Health Act, commonly referred to as the HITECH Act, markedly accelerated the uptake of electronic health records (EHR) systems within hospital settings, as demonstrated by an “increase in adoption figures from 3.2% before its enforcement to 14.2% subsequently, specifically among hospitals that met the eligibility criteria.”[xxxiii] Nevertheless, the scope of HITECH's incentives was primarily confined to hospitals providing short-term acute care, inadvertently omitting a significant portion of the healthcare ecosystem, including private practices, community health centers, and smaller medical establishments. These entities stand to gain considerably from the integration and enhanced functionality of EHR systems, particularly in terms of operational efficiency, patient care coordination, and cost reduction. This observation implies that while the HITECH Act has played a pivotal role in the digital transformation of certain healthcare facilities, its full potential remains untapped. Expanding its reach to encompass a broader spectrum of healthcare providers could magnify its positive impacts throughout the entire healthcare industry.
Accountable Care Organization (ACO) is a network of doctors and hospitals who agree to work together with Medicare and share responsibility for delivering high-quality, coordinated care to patients.[xxxiv] ACO is a value-driven healthcare delivery model that improves healthcare outcomes and lowers costs through improved coordination and efficient healthcare delivery (i.e., fewer unnecessary medical procedures, and coordinated preventative healthcare processes). Aledade, a startup established in 2014 and located in Bethesda, Maryland has been at the forefront of implementing a value-focused care strategy through its Accountable Care Organizations (ACOs) which effectively leverage technology and data analytics to assist primary care practices. By emphasizing care optimizing the management of chronic diseases and reducing unnecessary hospital visits Aledade’s model aims to enhance patient outcomes while simultaneously lowering healthcare expenses.[xxxv] Their innovative platform offers insights that enable practices to provide more efficient and personalized care.
One of the standout achievements of the Aledades ACO model is its record of cost savings and improved patient care. Specifically, Aledade delivered proactive preventative care to more than “1.15 million patients and saved more than $1.2 billion across the health care system over the past eight years.”[xxxvi] “These savings went straight to patients and their physicians alike, as practices working with Aledade are projected to have earned more than $167 million in shared savings payments for their work in 2021.”[xxxvii] These savings were made possible through decreases in hospital admissions and advancements, in both chronic disease management and the delivery of preventive healthcare services. This success highlights Aledade’s ability to achieve the objectives of value-based care; decreased costs and improved outcomes for patients.
D. Conclusion
As our exploration of the U.S. healthcare system's financial conundrums and operational labyrinths comes to a close, we reflect on the critical juncture at which the industry stands. Administrative complexity accounts for $265.6 billion in wasteful costs, according to a study published in JAMA.[xxxviii] With an annual healthcare expenditure that soared to $4.3 trillion in 2021, translating to an average of $12,900 per person,[xxxix] the economic pressure to redefine and rejuvenate healthcare delivery is immense. The challenge of administrative complexity, woven deeply into the fabric of healthcare operations, has been laid bare, revealing its costly tendrils that extend far beyond fiscal impact to influence the very quality of patient outcomes.
This series has illuminated a path forward, where innovation and ingenuity are key in unraveling the bureaucratic tape that constricts the healthcare system. The shift towards value-based care models heralds a future where patient outcomes are the North Star, guiding all efforts to streamline services and prune unnecessary administrative overhead. Technology, too, promises a revolution in efficiency, with EHRs and AI-driven tools standing ready to redefine the pace and precision of care delivery and insurance processing.[xl] It's within this innovative landscape that Aledade's ACO model shines, charting a course for the industry by proving that it's possible to marry financial savings with improved patient care—demonstrating in 2022 a stellar performance with over $1.5 billion in savings for Medicare.[xli] As we conclude, we are tasked with applying the lessons learned and insights gained toward developing a healthcare system that is financially prudent and steadfast in its dedication to patient care.
Notes (See bibliography for full citation of sources):
[i] Shrank, WH, TL Rogstad, and N Parekh. "Waste in the US Health Care System: Estimated Costs and Potential for Savings." JAMA 322, no. 15 (2019): 1501-1509. doi:10.1001/jama.2019.13978. Accessed March 2, 2024.
[ii] Peter G. Peterson Foundation. "Almost 25 Percent of Healthcare Spending Is Considered Wasteful — Here's Why." Peter G. Peterson Foundation. 2023. Accessed March 1, 2024. www.pgpf.org/blog/2023/04/almost-25-percent-of-healthcare-spending-is-considered-wasteful-heres-why.
[iii] Shrank, et. al, “Waste in the US Health Care System”
[iv] Ibid.
[v] Ibid.
[vi] Ibid.
[vii] "The Gathering Storm: The Uncertain Future of U.S. Healthcare." McKinsey & Company. September 16, 2022. Accessed March 1, 2024. www.mckinsey.com/industries/healthcare/our-insights/the-gathering-storm-the-uncertain-future-of-us-healthcare.
[viii] Ibid.
[ix] Ibid.
[x] McKinsey & Company, "The Gathering Storm: The Uncertain Future of U.S. Healthcare."
[xi] Shrank, et. al, “Waste in the US Health Care System”
[xii] McKinsey & Company, "The Gathering Storm: The Uncertain Future of U.S. Healthcare."
[xiii] Ibid.
[xiv] Ibid.
[xv] Ibid.
[xvi] Ibid.
[xvii] Ibid.
[xviii] Ibid.
[xix] Ibid.
[xx] Ibid.
[xxi] McKinsey & Company, "The Gathering Storm: The Uncertain Future of U.S. Healthcare."
[xxii] Ibid.
[xxiii] Peter G. Peterson Foundation. "Almost 25 Percent of Healthcare Spending Is Considered Wasteful — Here's Why."
[xxiv] Ibid.
[xxv] Tseng, Philip, et al. "Administrative Costs Associated with Physician Billing and Insurance-Related Activities at an Academic Health Care System." JAMA 319, no. 7 (2018): 691-697. Accessed March 3, 2024.
[xxvi] "The Impact of Administrative Complexity on Healthcare Costs and Quality." The American Journal of Managed Care. 2017. 21 no. 1 (2015): e1-e8. Accessed March 9, 2024.
[xxvii] Center for American Progress. "Excess Administrative Costs." Center for American Progres. 2019. Accessed March 3, 2024.
[xxviii] Tseng, Philip, et al. "Administrative Costs Associated with Physician Billing and Insurance-Related Activities at an Academic Health Care System."
[xxix] Erickson, Shari M., Brooke Rockwern, Michelle Koltov, and Robert M. McLean. "Putting Patients First by Reducing Administrative Tasks in Health Care: A Position Paper of the American College of Physicians." Annals of Internal Medicine. Published March 28, 2017. Accessed March 9, 2024. https://www.acpjournals.org/doi/10.7326/m16-2697.
[xxx] "Innovations in Healthcare Delivery: The Role of Technology and Integrated Systems." Health Affairs 33, no. 2 (2014): 244-251. Accessed March 1, 2024.
[xxxi] Adler-Milstein, Julia, and Ashish K. Jha. "HITECH Act Drove Large Gains In Hospital Electronic Health Record Adoption." Health Affairs 36, no. 8 (2017): 1416–1422. https://doi.org/10.1377/hlthaff.2016.1651. Accessed March 7, 2024.
[xxxii] Ibid.
[xxxiii] Ibid.
[xxxiv] Mount Sinai. "What is an ACO?" Mount Sinai. Accessed March 9, 2024. https://www.mountsinai.org/about/aco/what-is-an-aco.
[xxxv] “Aledade Has Saved More Than $1.2 Billion in Unnecessary Health Care Spending." Aledade. Accessed March 16, 2024. https://resources.aledade.com/home/aledade-has-saved-more-than-1-2-billion-in-unnecessary-health-care-spending/.
[xxxvi] Ibid.
[xxxvii] Ibid.
[xxxviii] Shrank, et. al. "Waste in the US Health Care System: Estimated Costs and Potential for Savings."
[xxxix] Peter G. Peterson Foundation. "Almost 25 Percent of Healthcare Spending Is Considered Wasteful—Here's Why."
[xl] Center for American Progress. "Excess Administrative Costs."
[xli] Aledade. "Aledade Has Saved More Than $1.2 Billion in Unnecessary Health Care Spending."
Bibliography
1. Shrank, WH, TL Rogstad, and N Parekh. "Waste in the US Health Care System: Estimated Costs and Potential for Savings." JAMA 322, no. 15 (2019): 1501-1509. doi:10.1001/jama.2019.13978. Accessed March 2, 2024.
2. Peter G. Peterson Foundation. "Almost 25 Percent of Healthcare Spending Is Considered Wasteful — Here's Why." Peter G. Peterson Foundation. 2023. Accessed March 1, 2024. www.pgpf.org/blog/2023/04/almost-25-percent-of-healthcare-spending-is-considered-wasteful-heres-why.
3. "The Gathering Storm: The Uncertain Future of U.S. Healthcare." McKinsey & Company. September 16, 2022. Accessed March 1, 2024. www.mckinsey.com/industries/healthcare/our-insights/the-gathering-storm-the-uncertain-future-of-us-healthcare.
4. Tseng, Philip, et al. "Administrative Costs Associated with Physician Billing and Insurance-related Activities at an Academic Health Care System." JAMA 319, no. 7 (2018): 691-697. Accessed March 3, 2024.
5. "The Impact of Administrative Complexity on Healthcare Costs and Quality." The American Journal of Managed Care. 2017. 21 no. 1 (2015): e1-e8. Accessed March 9, 2024.
6. Center for American Progress. "Excess Administrative Costs." Center for American Progres. 2019. Accessed March 3, 2024.
7. Erickson, Shari M., Brooke Rockwern, Michelle Koltov, and Robert M. McLean. "Putting Patients First by Reducing Administrative Tasks in Health Care: A Position Paper of the American College of Physicians." Annals of Internal Medicine. Published March 28, 2017. Accessed March 9, 2024. https://www.acpjournals.org/doi/10.7326/m16-2697.
8. "Innovations in Healthcare Delivery: The Role of Technology and Integrated Systems." Health Affairs 33, no. 2 (2014): 244-251. Accessed March 1, 2024.
9. Adler-Milstein, Julia, and Ashish K. Jha. "HITECH Act Drove Large Gains In Hospital Electronic Health Record Adoption." Health Affairs 36, no. 8 (2017): 1416–1422. https://doi.org/10.1377/hlthaff.2016.1651. Accessed March 7, 2024.
10. Mount Sinai. "What is an ACO?" Mount Sinai. Accessed March 9, 2024. https://www.mountsinai.org/about/aco/what-is-an-aco.
11. "Aledade Has Saved More Than $1.2 Billion in Unnecessary Health Care Spending." Aledade. https://resources.aledade.com/home/aledade-has-saved-more-than-1-2-billion-in-unnecessary-health-care-spending/. Accessed March 16, 2024.